Extracting A Root Canal Tooth
The relationship between a patient and their dentist is often founded on trust and the mutual goal of preserving oral health. In some cases, despite attempts to save a tooth through root canal therapy, the tooth may still face complications or become irreversibly damaged. As a result, the dentist might recommend the extraction of the affected tooth. While the prospect of having a previously treated tooth removed can be daunting, understanding the underlying reasons and the procedure itself can help alleviate concerns and ensure informed decision-making. This article aims to explore the circumstances in which a dentist might opt to remove a tooth that has undergone a root canal, shedding light on the process, potential complications, and post-extraction care.

What are the common reasons for a dentist to recommend the extraction of a tooth that has undergone a root canal procedure?
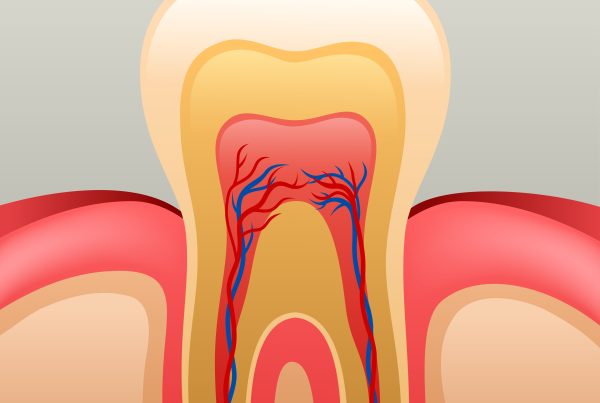
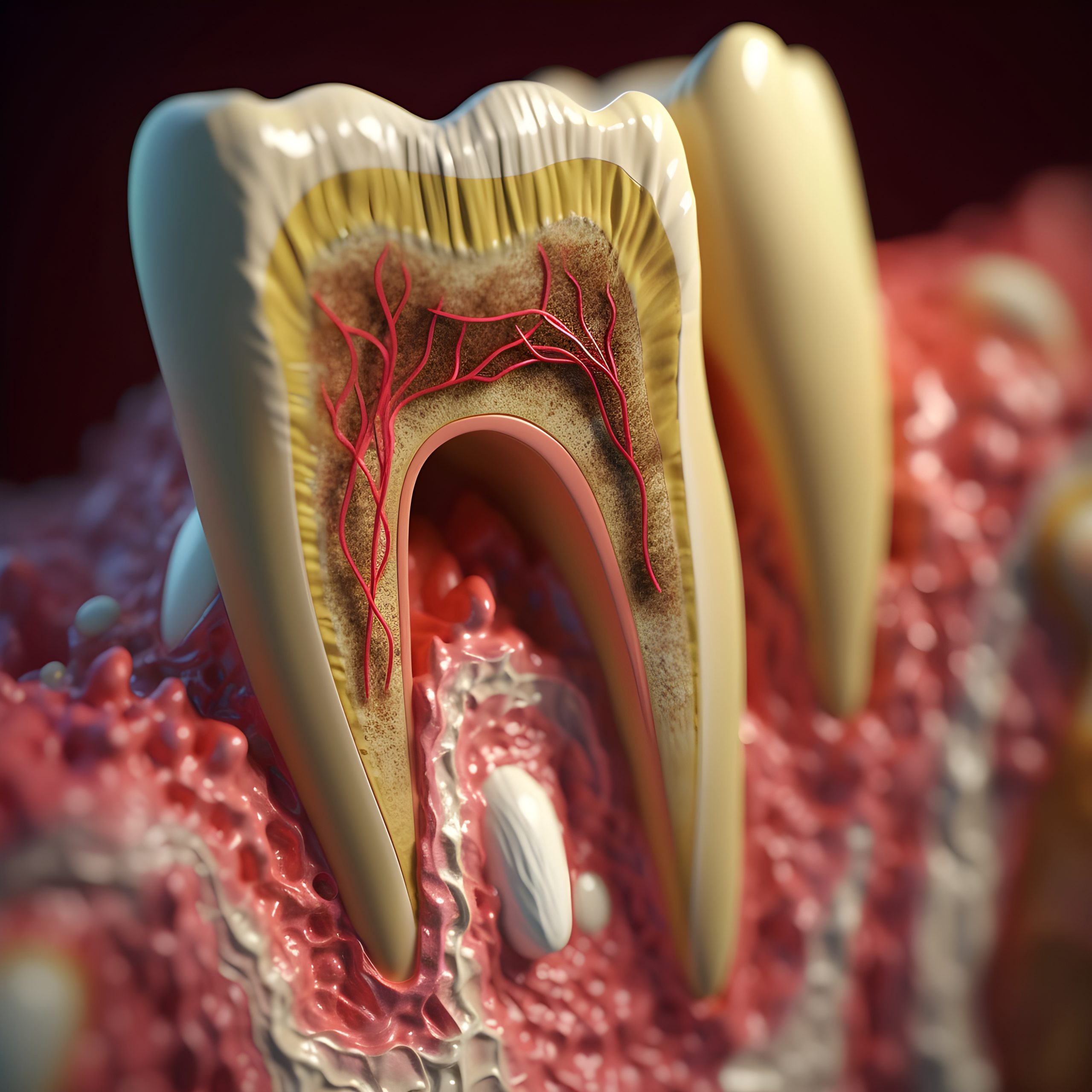
There are several reasons why a dentist might suggest the extraction of a tooth that has previously undergone a root canal procedure. One of the primary causes is the presence of persistent or recurrent infection. Despite the meticulous cleaning and sealing of the root canal during the initial treatment, certain cases may involve complex root structures or undetected additional canals that contribute to the re-emergence of an infection. In such instances, the infection can spread to the surrounding tissues and bone, leading to persistent discomfort, swelling, and even the formation of abscesses. As a result, the extraction of the tooth may be deemed necessary to prevent the infection from jeopardizing the overall oral health and to eliminate the source of persistent pain and inflammation.
Additionally, structural damage or fractures that compromise the integrity of the tooth may warrant its extraction following a root canal procedure. Despite the reinforced strength provided by a dental crown post-root canal, some teeth may experience fractures or cracks over time due to various factors such as trauma, bruxism (teeth grinding), or weakening of the tooth structure. Such damage can make the tooth vulnerable to further infection or make it difficult to restore the tooth effectively. Consequently, the dentist may recommend extraction as a means to eliminate the risk of continued complications and to explore alternative tooth replacement options that can restore functionality and maintain the structural integrity of the dental arch.
Can a general dentist remove a root canal tooth or do I need an oral surgeon?
In many cases, a general dentist can perform the extraction of a root canal-treated tooth. General dentists are trained to handle a variety of dental procedures, including tooth extractions, and they often have the necessary skills and experience to remove a tooth effectively. However, there are certain situations where the complexity of the extraction or the patient’s specific needs may necessitate the expertise of an oral surgeon.
If the tooth is severely impacted, positioned in a way that makes it challenging to access, or if the patient has complex medical conditions that require special considerations, an oral surgeon may be recommended. Oral surgeons have advanced training in a range of oral and maxillofacial surgical procedures, including complex tooth extractions. They are equipped to handle more complicated cases and can provide specialized care for patients with specific needs, ensuring a higher level of expertise and precision during the extraction process.
Ultimately, the decision regarding whether a general dentist or an oral surgeon should perform the extraction of a root canal-treated tooth depends on the complexity of the case, the dentist’s comfort level with the procedure, and the patient’s individual circumstances. Your dentist will assess your specific situation and determine the most appropriate course of action to ensure a successful and comfortable treatment outcome.

How does a dentist determine whether a root canal tooth should be extracted or preserved?
A dentist will typically consider various factors to determine whether a root canal-treated tooth should be preserved or extracted. These factors may include the extent of the tooth’s structural damage, the presence of any recurrent infections, the overall health of the surrounding gums and bone, and the patient’s general oral health and medical history. They will conduct a thorough clinical examination, which may involve X-rays or other imaging techniques to assess the condition of the tooth’s root and surrounding structures. Additionally, the dentist will evaluate the potential success of retreatment options or alternative restorative procedures, weighing the benefits and risks of preserving the tooth against the potential complications that may arise if the tooth is retained. By considering all these aspects, the dentist can make an informed decision tailored to the patient’s specific needs and long-term oral health goals.
What are the potential complications that may arise during or after the extraction of a root canal-treated tooth?
The extraction of a root canal-treated tooth, while generally a routine dental procedure, can still pose certain potential complications. These complications may include excessive bleeding during or after the extraction, especially if the patient has a bleeding disorder or is taking blood-thinning medications. Additionally, there is a risk of infection at the extraction site, which can lead to delayed healing and potentially more severe complications if left untreated. Damage to nearby teeth, nerves, or the surrounding bone can occur during the extraction process, resulting in prolonged discomfort, numbness, or altered sensation in the mouth or surrounding areas. Furthermore, there is a possibility of developing a condition known as dry socket, where the blood clot at the extraction site dislodges prematurely, leading to intense pain and delayed healing. Patients may also experience swelling, bruising, or temporary difficulty opening the mouth fully due to inflammation and trauma to the surrounding tissues. It is important for patients to closely follow post-extraction care instructions provided by the dentist to minimize these potential complications and promote optimal healing.


How does the process of extracting a root canal-treated tooth differ from that of extracting a non-treated tooth?
The process of extracting a root canal-treated tooth may differ from that of extracting a non-treated tooth primarily in the structural complexity and potential fragility of the treated tooth. During the extraction of a root canal-treated tooth, the dentist must consider the presence of any remaining filling materials, posts, or other restorative elements within the tooth that may complicate the extraction process. These additional materials may require careful manipulation or removal to ensure the complete extraction of the entire tooth, including its roots. The treated tooth, especially if it has undergone significant structural weakening or has experienced fractures, may be more fragile and prone to breakage during the extraction procedure, necessitating careful handling to prevent complications such as retained root fragments or damage to the surrounding tissues.
In contrast, the extraction of a non-treated tooth typically involves the straightforward removal of the tooth from its socket without the need to navigate through any previously placed filling materials or restorations. Non-treated teeth generally have their natural structure intact, which may make the extraction process relatively simpler and more predictable compared to that of a root canal-treated tooth. However, it’s essential to note that the specifics of the extraction procedure can vary depending on the individual circumstances of the patient and the tooth in question. The dentist will carefully evaluate the unique characteristics of each case to determine the most appropriate approach for a successful and efficient extraction.