Root Canal Treatment Length
A root canal is a dental procedure designed to address issues within the soft pulp of a tooth, such as infection or damage. While the duration of a root canal can vary based on several factors, including the tooth's location, complexity of the case, and the patient's individual circumstances, the procedure generally takes one to two hours to complete. Root canals are performed by dentists or endodontists, who specialize in the treatment of dental pulp. Despite common misconceptions about their discomfort, modern advancements in dental technology and anesthesia make root canals a relatively routine and often pain-free procedure, crucial for salvaging a damaged tooth and alleviating associated pain or infection. Understanding the factors influencing the duration of a root canal can provide individuals with a clearer perspective on what to expect during this essential dental intervention.

Who performs a root canal?
A root canal is typically performed by a dentist or an endodontist. Both dentists and endodontists have the necessary training to carry out this dental procedure, but endodontists are specialists with additional education and expertise specifically focused on the diagnosis and treatment of issues related to the dental pulp and the inner parts of the tooth.
In many cases, a general dentist will be the first to diagnose the need for a root canal during a routine dental examination. If the case is straightforward, the general dentist may perform the root canal. However, if the situation is more complex, or if the patient prefers to see a specialist, the dentist may refer the patient to an endodontist.
Endodontists are dental specialists who have completed additional training, usually two or more years beyond dental school, to become experts in treating the dental pulp and performing root canal procedures. They are equipped to handle challenging cases and are particularly skilled in managing the intricacies of root canal therapy. The choice between a general dentist and an endodontist often depends on the complexity of the case and the patient’s preferences.
What is the root canal procedure like?
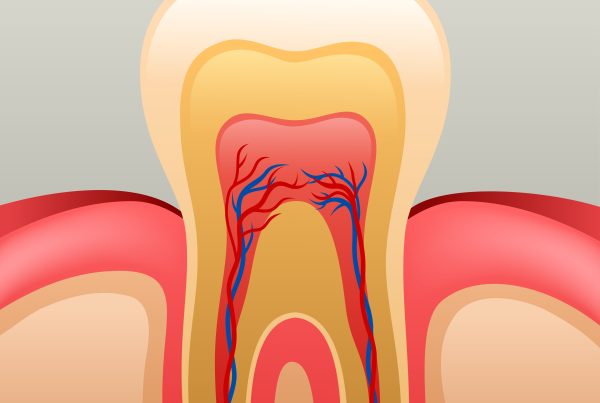
The root canal procedure is a dental treatment aimed at addressing issues within the pulp of a tooth, such as infection or damage. Here is a general overview of what the root canal process involves:
- Diagnosis and X-rays: The dentist or endodontist begins by examining the tooth and taking X-rays to assess the extent of the issue. This helps in determining the shape of the root canals and identifying any signs of infection or damage.
- Local Anesthesia: Before starting the procedure, the dentist administers local anesthesia to ensure the patient is comfortable and does not feel pain during the root canal.
- Isolation of the Tooth: The dentist places a rubber dam around the affected tooth to keep it dry and free from saliva during the procedure.
- Access Opening: The dentist creates a small opening in the crown of the tooth to access the pulp chamber and root canals.
- Pulp Removal: The infected or damaged pulp is carefully removed from the pulp chamber and each of the root canals using specialized instruments. The interior of the tooth is then cleaned and shaped to prepare it for filling.
- Cleaning and Shaping: The dentist uses small files to clean and shape the inside of the tooth, ensuring that all traces of pulp and debris are removed.
- Irrigation: The dentist irrigates the canals with a solution to disinfect and flush out any remaining debris.
- Filling: Once the canals are clean, they are filled with a biocompatible material called gutta-percha to seal them and prevent further infection.
- Temporary or Permanent Restoration: Depending on the case, the dentist may place a temporary or permanent filling to seal the access opening. In some cases, a crown may be recommended to provide additional protection and restore the tooth’s functionality.
- Follow-up: After the root canal, the patient may need to schedule a follow-up appointment to monitor the healing process. In some cases, a permanent restoration like a crown may be placed in a subsequent appointment.
While the term “root canal” often invokes fear, advancements in dental technology and anesthesia have made the procedure more comfortable than its reputation suggests. Patients typically experience relief from pain and discomfort following a successful root canal, as the treatment effectively addresses the underlying dental issues.


Is a root canal painful?
The perception of pain during a root canal has been a common concern, but with modern advancements in dental techniques and anesthesia, the procedure is typically not as painful as its reputation suggests. In fact, the primary goal of a root canal is to alleviate pain and discomfort caused by an infected or damaged tooth.
Here’s why a root canal is generally not as painful as people might fear:
- Local Anesthesia: Before starting the root canal procedure, the dentist or endodontist administers a local anesthetic to numb the affected tooth and the surrounding area. This ensures that the patient does not feel pain during the treatment.
- Technological Advancements: Dental technology has significantly improved, allowing for more precise and efficient root canal procedures. Advanced instruments and techniques contribute to minimizing discomfort and shortening the duration of the treatment.
- Dentist’s Expertise: Dentists and endodontists are trained professionals with the expertise to perform root canals efficiently and with a focus on patient comfort. Their skill and experience contribute to a smoother and less painful experience for the patient.
- Post-Procedure Care: After the root canal, any discomfort or pain is usually manageable with over-the-counter pain medications. The intense pain that may have prompted the need for the root canal is typically relieved by the procedure itself.
It’s essential for patients to communicate openly with their dentist about any concerns or anxiety they may have. Dentists can provide additional sedation options or discuss strategies to help manage anxiety during the procedure.
While individual experiences may vary, many people find that the pain associated with a root canal is often exaggerated, and the procedure itself is a crucial step in preserving a tooth and eliminating the underlying source of pain. In the hands of a skilled and experienced dental professional, a root canal can be a relatively routine and painless process.
The duration of a root canal procedure can vary depending on various factors, including the tooth’s location, the complexity of the case, and the individual patient’s circumstances. On average, a root canal procedure typically takes one to two hours to complete. However, it’s important to note that this is a general estimate, and actual time can vary.
Here are some factors that can influence the length of a root canal procedure:
- Tooth Location: The location of the tooth in the mouth can impact the complexity of the procedure. Front teeth usually have fewer and more straightforward roots, making the process quicker than molars, which often have multiple roots and can be more challenging to access.
- Number of Canals: The number of root canals within a tooth also affects the procedure’s duration. Teeth can have varying numbers of canals, and the dentist needs to clean and fill each one thoroughly.
- Severity of the Infection or Damage: The extent of infection or damage to the tooth’s pulp can influence the time required for the procedure. Severe cases may demand more meticulous cleaning and shaping.
- Patient Factors: Individual patient factors, such as the patient’s anatomy, response to anesthesia, and cooperation during the procedure, can impact the overall time needed.
- Temporary or Permanent Restoration: Depending on the case, the dentist may place a temporary filling or a permanent restoration (like a crown) during the same appointment or schedule a follow-up appointment for the restoration. This can add to the overall time spent at the dental office.
It’s essential to discuss the estimated duration of the root canal procedure with your dentist beforehand. They can provide insights based on your specific case and help manage expectations. While the root canal process is often completed in a single visit, complex cases or the need for additional procedures may extend the treatment timeline.


Are root canals necessary?
Root canals are necessary when the dental pulp, which contains nerves, blood vessels, and connective tissue within a tooth, becomes infected or damaged. This can occur due to deep decay, trauma, repeated dental procedures, or cracks in the tooth. Without intervention, the infection can spread, leading to severe pain, abscess formation, and potential tooth loss. A root canal procedure involves removing the infected or damaged pulp, cleaning and shaping the interior of the tooth, and sealing it to prevent further infection. While the reputation of root canals may evoke apprehension, they are essential for preserving a tooth, alleviating pain, and preventing the spread of infection to neighboring teeth or other parts of the body. Advances in dental technology and anesthesia have made root canals more comfortable, and the procedure is often the most effective way to save a tooth from extraction.
Can a root canal fail?
Yes, a root canal can, on rare occasions, fail to completely resolve the issues within a tooth. A root canal failure may occur for several reasons:
- Incomplete Removal of Infected Tissue: If the dentist or endodontist does not thoroughly remove all of the infected or damaged pulp during the root canal procedure, bacteria can persist and cause a new infection.
- Complex Anatomy: Some teeth have intricate canal systems that may be challenging to completely clean and seal. Undetected or untreated accessory canals can lead to persistent or recurrent infections.
- Undetected Cracks or Fractures: A tooth with an undetected crack or fracture may not respond successfully to a root canal. Cracks can allow bacteria to enter and cause reinfection.
- Insufficient Restoration: After a root canal, the tooth needs a proper restoration, usually with a crown, to prevent recontamination and provide structural support. If the restoration is inadequate or delayed, the tooth may be at risk of failure.
- New Trauma or Decay: Subsequent trauma or new decay to a tooth that has undergone a root canal can compromise its success.
- Unresolved Periapical Lesion: If a lesion or infection around the root of the tooth persists after the root canal, it may indicate a failure.
In the event of a failed root canal, retreatment or endodontic surgery (apicoectomy) may be considered to address the underlying issue. In some cases, extraction of the tooth and replacement with a dental implant or bridge may be necessary. It’s important for individuals to attend follow-up appointments, report any unusual symptoms, and maintain good oral hygiene to maximize the success of root canal treatments. Additionally, early detection and intervention contribute significantly to the overall success of root canal procedures.


Root canal treatment at Best Dental
Receiving root canal treatment at Best Dental with Dr. Sonny Naderi promises an exceptional and patient-centered experience. Dr. Naderi, renowned for his expertise and commitment to dental care, ensures a meticulous and comfortable root canal procedure. With state-of-the-art facilities and advanced dental technology, Best Dental provides a cutting-edge environment for diagnosis, treatment, and aftercare. Dr. Naderi’s personalized approach and attention to detail prioritize patient well-being, addressing any concerns and ensuring a pain-free experience through the use of the latest anesthetic techniques. Patients can trust in the proficiency of Dr. Naderi and the Best Dental team, knowing that their root canal treatment is in the hands of a skilled professional dedicated to achieving optimal oral health outcomes.